This week we are having a guest article by Alexandra Johansson and Kirsty Toms
Have you ever visited your doctor thinking that you may need antibiotics? Here are some facts about whether you may or may not need these popular pills and why they aren’t the solution to everything.
WHAT ARE ANTIBIOTICS?
Infections are caused by tiny bugs such as bacteria, viruses, fungi and parasites. These bugs are all very different from each other in shape, size and structure. Therefor, different medicines are needed to treat each one. The term antibiotic is usually used to describe a medicine which destroys or paralyses bacteria, so that they can no longer harm you. They will have no effect on a fungal infection (where an anti-fungal is needed) or a viral infection (where an anti-viral medicine is needed, that is if one exists).
WHAT TYPES OF ANTIBIOTICS ARE THERE?
Antibiotics can be divided into two types – narrow-spectrum and broad-spectrum. Narrow-spectrum antibiotics are extremely specific – they may only target one or two different bacteria. They are useful when your doctor knows which bacteria is causing an infection.
In the earlier stages of an infection it may be impossible to identify the exact bacteria and a broad-spectrum antibiotic might be used. These are effective in killing a wide range of bacteria. The idea of an antibiotic which wipes out all bacteria sounds excellent, but it is important to mention that not all the bacteria in our bodies are bad!! For example, we are quite reliant on bacteria in our gut to process food, form stools and fight off invading bacteria. When a broad-spectrum antibiotic comes along and kills these good bacteria, bad bugs can take over and cause serious infections such as C.Difficile.
WHEN SHOULD ANTIBIOTICS BE USED?
There are many situations where antibiotics are extremely effective and also life-saving, for example in illnesses like meningitis and blood poisoning. They may be used alone or in combination in more severe infections. As part of our medical training we are taught how to determine which infections are likely to be bacterial based on your symptoms. Doctors can test your blood, urine, stools or spit to find out the exact bug causing an infection and which antibiotics will work for your particular bug. This may take a couple of days.
WHEN ARE ANTIBIOTICS NOT USEFUL?
It might sound obvious but if you don’t have a bacterial infection then you do not need antibiotics! Conditions such as the common cold are caused by viruses, so taking an antibiotic won’t help your symptoms. If you’ve ever had antibiotics for a cold, you may have felt better over a couple of days but this is your own body’s immune system kicking in and making you well. It is not because of the antibiotics!
It is also important to note that many antibiotics come with side effects, the most common being diarrhoea. That is not something most people would appreciate for no good reason!
WHAT IS ANTIBIOTIC RESISTANCE?
Antibiotic resistance occurs when bacteria find clever ways to escape the effects of antibiotics which used to be able to kill them. When an antibiotic kills all bacteria but those that are resistant, the resistant bacteria are left to thrive without any competition. This phenomenon increases the more we use antibiotics.
WHAT’S THE PROBLEM WITH ANTIBIOTIC RESISTANCE?
When bugs become resistant to antibiotics it means doctors are left with fewer antibiotics to choose from. This becomes even more of a problem if you are allergic to certain antibiotics or the bug is resistant to multiple antibiotics. The remaining antibiotics may also have nastier side effects! We may run out of antibiotics all together quite soon…
IS ANTIBIOTIC RESISTANCE A PROBLEM EVERYWHERE?
Yes!!
In the UK we are seeing alarming numbers of ‘superbugs’ such as MRSA, which are resistant to many different antibiotics. This is because we have a long history of doctors prescribing antibiotics when they are not needed and patients not taking the correct course of medication.
There has been little research done on antibiotic resistance in Dominica, but it appears to be a fast-growing problem.
WHAT CAN YOU DO?
Patients can help by only taking antibiotics that have been prescribed to them by their doctor and completing the full course of medicine. Even if you feel better, it is important to take all of the tablets! It is also crucial not to share your antibiotics with anyone else. That means no taking your grandmother’s leftovers, as you would not be getting a full course and you may be contributing to antibiotic resistance.
Doctors can help by only prescribing antibiotics when they are truly needed and making absolutely sure they are using the most appropriate antibiotic for an infection. It can be very difficult for doctors to say no to their valued patients when they ask for antibiotics, even if it goes against their better judgement.
The government can also help by recording data on which bacteria are resistant and putting money into developing new antibiotics.
CONCLUSION
Antibiotic resistance is a big problem and everyone can help by only taking antibiotics when they are really needed!
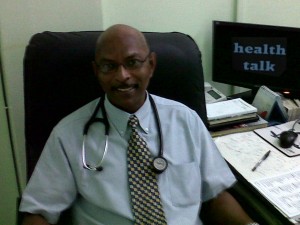
Alexandra Johansson and Kirsty Toms are medical students at the University of Glasgow in Scotland, on attachment with Dr. Emanuel for the month of August.
See you next week.

Thanks Dr. Emanuel, Alexandra and Kirsty. I don`t like antibiotic. It messed-up my hair some years ago, from that I dislike taking it.
This was a wonderful job by two obviously well-schooled young ladies.
I think they chose the right doctor to do an attachment with too.
Good summary, girls. Well done. I am currently enjoying my locum at the Victoria Infirmary in your base city